Our Impact in Numbers
funded in 2024
funded in 2024
received in 2024
donors in 2024
distributed for 2025
therapy programs since 2012
funded since 2012
since 2012
2024 Program Demographics
40%
78%
91%
89%
54%
83%
57%
57%
40%
24%
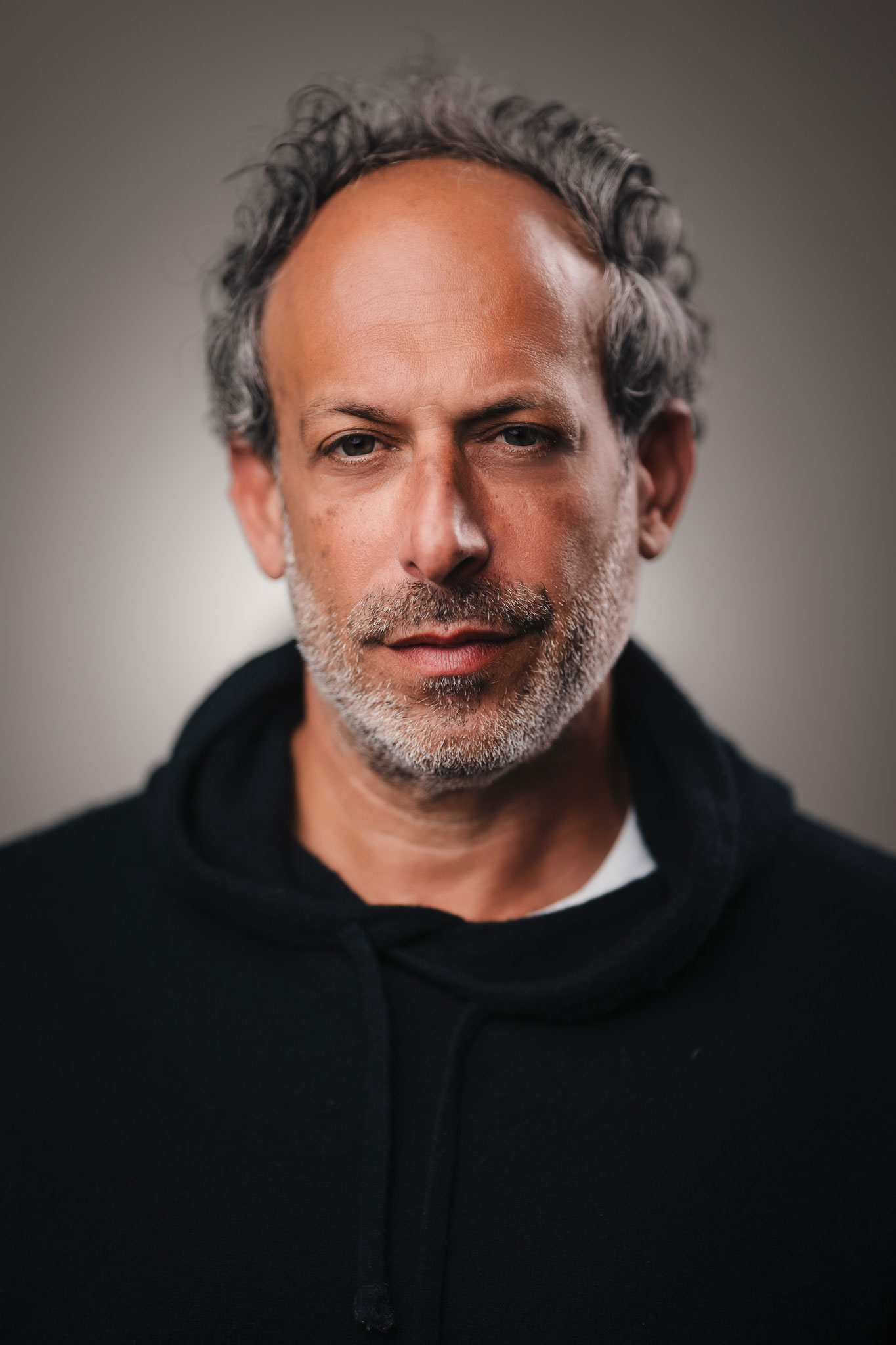
A Message from Board President, David Barnett
Our mission at Music Heals is to help spread awareness and raise funds for the power that music plays on our mental, physical, and spiritual health. We know that music helps us with our psychological, emotional, and social needs by helping us work through whatever we are going through.
As we continue to provide a huge need in our community, funding facilities that believe in the power of music as medicine, we continue to see a growing need for Music Therapy programs throughout the lower mainland and across the province.
The medicine is really in the music. And more than ever we need that medicine.
Thank you to everyone who continues to support our cause,
David Barnett
A Message from Executive Director, Juliana Fraser
Through the support of our generous donors and sponsors, we provided funding to 37 music therapy programs across British Columbia in 2024. I have had the privilege of touring some of these facilities over the past year and I can tell you first-hand, we are making a difference in the lives of people of all ages benefitting from music therapy. Music is truly changing lives!
From people undergoing cancer treatment, using music therapy to provide them with a calming resource to process their fears and trauma, to at-risk children on the Downtown Eastside having access to music therapy to support the development of language and social skills to prepare them for kindergarten, music is being used as a tool for healing.
I am honoured to share some of these stories with you here in our 2024 Annual Report. The power of music is seen every day in the lives of people of all ages who are benefitting from music therapy and I look forward to continuing to share their stories with you.
Sincerely,
Juliana Fraser

Changing Lives Through Music
Music Heals Charitable Foundation believes in the healing power of music. We provide crucial funding to music therapy programs across BC giving the gift of music to those who need it most.
Funded Facilities 2024
See below for some incredible stories of the Impact of Music Therapy from a number of these programs & facilities
- To donate to music heals, including a dedicated donation to one of the programs above, click here to Make a Donation
For more information of any of the programs or demographics supported through donations to Music Heals, reach out to us at info@musicheals.ca
Let Her Sing 2024
Together we raised over $120,000 for music therapy programs for women
Our 4th annual fundraising luncheon held Tuesday, March 5, 2024, the week of International Women’s Day was a remarkable success in raising vital funds for music therapy programs supporting women’s mental health, addiction recovery, and women working in the street-based sex trade on the DTES.
This wouldn’t have been possible without the unwavering support of our incredible sponsors, event partners, gift bag donors, shopping vendors and guests who joined us in making the afternoon so memorable.
38th Annual ZLC Foundation Charity Golf Tournament
Thank you ZLC Foundation for raising $70,000 for Music Heals!
A huge thank you to ZLC Foundation for choosing Music Heals as the beneficiary of the 38th Annual ZLC Foundation Charity Golf Tournament held on July 8, 2024, at Richmond Country Club.
We had a fantastic day and want to extend our deepest gratitude to the team at ZLC, the golfers, the donors as well as the event partners who helped to make this event possible.
It was an incredible day of golf, music and sunshine all in support of raising funds and awareness for music therapy across BC.
A Benefit for Music Heals 2024
An unforgettable evening celebrating the power of music, and raising over $450,000 for music therapy programs in 2025
Our annual gala, A Benefit for Music Heals held on Thursday, October 17, 2024, was once again a remarkable success in raising crucial funds to support the therapeutic use of music in physical and mental health practices across British Columbia.
This would not have been possible without the unwavering support of our incredible sponsors, table hosts, event partners, generous donors, and guests who joined us in making the evening spectacular. To all of you, we extend a massive thank you!
#GivingTuesday 2024
One Note at a Time. One Post at a Time. One Donation at a Time. Together, you helped us to change lives through music!
GivingTuesday is a global generosity movement unleashing the power of people and organizations to transform their communities and the world.
Click to watch this special version of Stand By Me recorded by some incredibly talented artists for our GivingTuesday campaign. The video has been viewed over 6000 times! Thank you for coming together to share the power of music!
Community Fundraisers in 2024
Fundraising initiatives hosted by amazing supporters of Music Heals
SEASKY EVENTS 80'S BIG FUN RUN
$350 in donations to Music Heals
KITCHEN TABLE RESTAURANTS
$1560 in donations to Music Heals
AMELIA'S 10TH BIRTHDAY PARTY
$450 in donations to Music Heals
CHARITY POKER TOURNAMENT IN MEMORY OF ANTHONY LLOYD KENNEDY
$800 in donations to Music Heals
ST. GEORGE'S UNITED CHURCH
$1740 in donations to Music Heals
EARL HAIG SECONDARY SCHOOL MUSIC DEPARTMENT
$1200 in donations to Music Heals
WEST SIDE MUSIC TOGETHER
$360 in donations to Music Heals
Wishlist Foundation
$1200 in donations to Music Heals
Misch
$2450 in donations to Music Heals
Sprouts Academy
$700 in donations to Music Heals
Salmon Arm Folk Fest
$2300 in donations to Music Heals
Paula Toledo & The Lost Song Community
$1000 in donations to Music Heals
- THANK YOU TO EVERYONE WHO ORGANIZED A FUNDRAISING INITIATIVE FOR MUSIC HEALS IN 2024
Together you have not only helped to provide crucial funding support for music therapy programs for people of all ages but you're helping us in our mission to increase awareness for music therapy as well by sharing our cause with your network, friends & family members.
CLICK HERE FOR MORE INFORMATION ON CREATING YOUR OWN FUNDRAISING INITIATIVE FOR MUSIC HEALS
2024 Amplify Donors






- Huscroft Family Charitable Trust
- Lynne Taylor Fund
- The Lawson Foundation
- MakeWay Foundation - Dr. Bik May Wai & Dr. Chung Nin Lam Endowment
Thank you to all our donors, sponsors and partners in 2024 for helping us give the gift of music to vulnerable people in need through increasing access to music therapy programming across British Columbia.
TOGETHER WITH YOUR GENEROUS SUPPORT, WE ARE CHANGING LIVES THROUGH MUSIC.
CLICK HERE FOR MORE INFORMATION ON SPONSORSHIPS AND CORPORATE GIVING